A Picture Is Worth a Thousand Words: Using Storyboards to Humanize the COVID-19 ICU Experience
By: Jennifer LaCoss, MD
January 4, 2021
In medicine, we value the connections that we forge with our patients as we walk alongside them—getting to know them, understand them, and learn what they value and how they live. In the ICU, when patients are unable to speak for themselves, a close substitute may be a spouse, family member, or friend at the bedside. Day by day, they weave together pieces of the fabric of their loved one’s life, telling us cherished stories and details that are important for us to know as we care for people.
As a palliative care physician, I hold tremendous value in these encounters with patients and families. They tell me they were not always the frail, chronically ill person in the ICU, but once a strong, vibrant marathon runner, farmer, or teacher; they explain what they enjoy and how their days were spent. The families also tell a narrative of hobbies, holidays, and milestones. As caregivers and clinicians, we remember these elements and craft a meaningful plan for each patient. It may be as simple as turning on the TV to a favorite show or as critical as knowing that they hope to live long enough to see a child get married.
The COVID-19 pandemic has dramatically changed the landscape of how we care for our patients. This virus has raged on, forcing hospitals to lock down in an effort to stem the rising tide. Gone are the days when I could sit next to an intubated person in the ICU, learning about my patient from family members or friends. Hospital systems have determined that it is no longer safe for visitors to be present hour by hour, day by day.
Proning has become a core part of care for patients with lungs ravaged by COVID-19. Laying a patient on their stomach further dehumanizes them and limits the opportunity to see and know them. It has become routine to round on room after room, with patients laying on their stomachs, indistinguishable from the human in the next room. Dehumanization is followed by demoralization of the care teams, who show up to fight for these patients every day. Vital signs and labs are still there, but the narratives, birthdays, anniversaries, worries, and hopes are starkly absent. Phone conversations with loved ones help, but are poor substitutes.
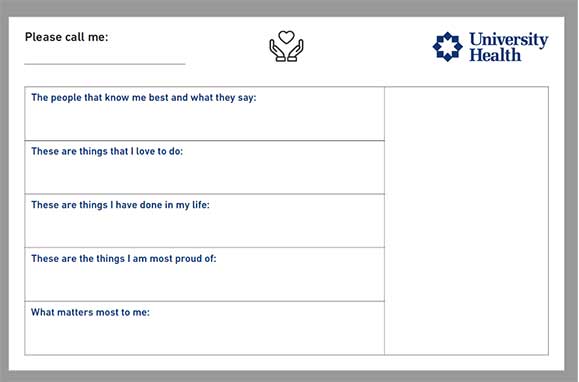
As we navigate this changed landscape, we must find other ways to create connections with our patients. One way is to recruit family and friends to provide those narrative elements and create a storyboard. This is an elegantly simple solution to a complicated problem. A storyboard can contain those important things that a patient might want us to know and also provide an opportunity to feature photos of the patient.
The benefits go both ways. Medical teams get to know a patient and see who they are, and family members feel more connected and cared for in the process. Each time I receive information for a storyboard from a family, it is accompanied by gratitude. It reinforces the faith that their loved one is in caring hands and provides a reminder that we are still trying. The storyboards are just as meaningful for staff, offering important details and a glimpse into the life that we are caring for, renewing the sense of connection to our patients. These storyboards provide an anchor in this turbulent storm, reminding us why we show up every day.
Dr. LaCoss would like to recognize Kelly Ferraro, MD, Palliative Medicine Attending at the Denver Health and Hospital Authority, Holly Keyt, MD, FCCP, Medical Director of the Adult Cystic Fibrosis Center at UT Health San Antonio, and Al Gonzalez, Patient Relations at University Hospital in San Antonio, for their support and assistance with this project.
Sample Storyboard

Jennifer LaCoss, MD, is an Assistant Professor of Medicine at UT Health San Antonio and Medical Director of Palliative Care at University Health System in San Antonio, Texas.